3D cell culture as a suitable research platform for multiple sclerosis (MS)
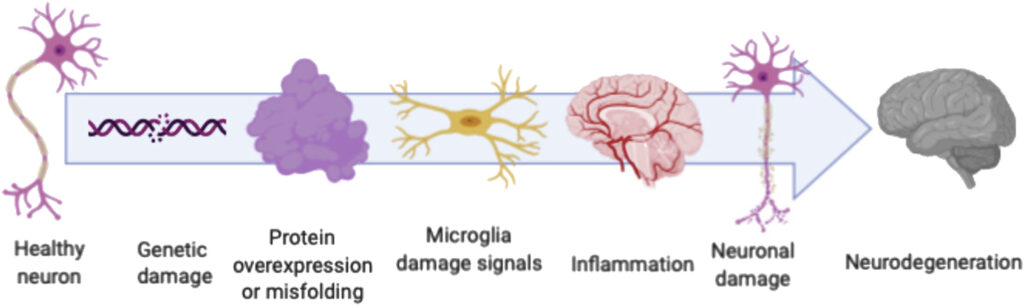
Among the neurodegenerative diseases, MS is the most common chronic disease prevalent among the young adult population with an early onset at 20-40 years of age, with a high occurrence among women (1). MS is characterized by focal plaques with demyelinated axons, proliferating astrocytes, activated microglia, lymphocytic and macrophage infiltration and decline of oligodendrocytes (2-3). These pathological events ultimately cause severe motor dysfunction, fatigue, tremors, nytagmus, acute paralysis, loss of balance, numbness, disrupted speech and vision, and eventual cognitive decline. MS is multifactorial in its etiology, and treatment options include drugs that encourage remyelination of damaged axons, to help with the degenerative stage of MS (4).
Rodent 3D organotypic slices
Given the complex mechanisms involved in the progression of MS, 3D cell cultures are accepted as a reliable research model. Most 2D monolayer cultures are unable to recapitulate the 3D cellular architecture of neurons, with its cellular microenvironment. Rodent 3D organotypic slices are commonly used to this effect, as it contains multiple regions of central nervous system, and can be maintained for several months thus allowing researchers to study the progression of axon myelination (5). Introducing toxins or an immune challenge can induce demyelination of axons. The reproducibility of this system also makes it an excellent platform to screen for potential drugs that induces remyelination (6).
Although rodent organotypic slices have yielded promising results, several therapeutic compounds tested on this system have proved unsuccessful in human trials, highlighting a major limitation of animal models at accurately representing human disease (7). This further confirms the need for new 3D in vitro tools to adequately mimic the human MS phenotype and subsequently identify possible therapeutic targets.
Human oligodendrocyte based 3D cultures– a promise of personalized medicine
3D cultures derived from human oligodendrocytes or oligodendrocyte precursors cells (OPCs) were developed as an attempt to overcome the limitations posed by animal models. They are usually generated using human embryonic stem cells, iPSCs, fetal cortical neurospheroid-derived cells, or umbilical cord derived stem cells (8,9). Stem cell use also introduces the possibility of 3D cultures based on patient specific cells, thus providing a platform to test for genetic variations, and subsequently personalized treatment options (10).
References
1. Compston, A., and Coles, A. (2008). Multiple sclerosis. Lancet 372, 1502–1517.
2. Stys, P. K., and Tsutsui, S. (2019). Recent advances in understanding multiple sclerosis. F1000Res. 8:F1000 Faculty Rev-2100.
3. Huang, W. J., Chen, W. W., and Zhang, X. (2017). Multiple sclerosis: pathology, diagnosis and treatments. Exp. Ther. Med. 13, 3163–3166.
4. Ghasemi, N., Razavi, S., and Nikzad, E. (2017). Multiple sclerosis: pathogenesis, symptoms, diagnoses and cell-based therapy. Cell J. 19, 1–10.
5. Schnadelbach, O., Ozen, I., Blaschuk, O. W., Meyer, R. L., and Fawcett, J. W. (2001). N-cadherin is involved in axon-oligodendrocyte contact and myelination. Mol. Cell. Neurosci. 17, 1084–1093.
6. Tan, G. A., Furber, K. L., Thangaraj, M. P., Sobchishin, L., Doucette, J. R., and Nazarali, A. J. (2018). Organotypic cultures from the adult CNS: a novel model to study demyelination and remyelination ex vivo. Cell. Mol. Neurobiol. 38, 317–328.
7. t Hart, B. A., Gran, B., and Weissert, R. (2011). EAE: imperfect but useful models of multiple sclerosis. Trends Mol. Med. 17, 119–125.
8. Bechler, M. E., Byrne, L., and Ffrench-Constant, C. (2015). CNS myelin sheath lengths are an intrinsic property of oligodendrocytes. Curr. Biol. 25, 2411–2416.
9. Leite, C., Silva, N. T., Mendes, S., Ribeiro, A., De Faria, J. P., Lourenco, T., et al. (2014). Differentiation of human umbilical cord matrix mesenchymal stem cells into neural-like progenitor cells and maturation into an oligodendroglial-like lineage. PLoS One 9:e111059.
10. Di Ruscio, A., Patti, F., Welner, R. S., Tenen, D. G., and Amabile, G. (2015). Multiple sclerosis: getting personal with induced pluripotent stem cells. Cell Death Dis. 6:e1806.
11. Valeria Valadez-Barba, A. Cota-Coronado, O.R. Hernández-Pérez, Pavel H. Lugo-Fabres, Eduardo Padilla-Camberos, Néstor Fabián Díaz, N. Emmanuel Díaz-Martínez. (2020) iPSC for modeling neurodegenerative disorders, Regenerative Therapy,Volume 15, Pages 332-339.
