Breakthroughs in glioblastoma research with neurosphere
Glioblastoma (GBM) is considered as among the most severe tumours across cancer types, and among brain tumours is considered most lethal. At present glioblastomas are incurable. These are aggressive tumours, infiltrating healthy neural tissues to the point of rendering surgical removal impossible. Currently therapeutic measure include surgery to remove as much of the cancer tissue as possible, followed by chemoradiotherapy to treat the remainder of tumour cells. Despite these treatment the average survival period remains at 14.5 months, and regardless of the success of the treatment, these tumours almost, always recur (1,2).
The challenges in glioblastoma research lies in the lack of a proper research platform. Presently, the patients themselves are the most reliable test bed, albeit, by the time the tumour is found, it is often progressed, and may even have evolved to develop treatment resistance. The heterogeneity of the tumour itself, further complicates any attempts to gain insight, into tumour progression and function. The most efficient method to combat these challenges is to develop an in-vitro model, that can be probed in the lab, where progression of the tumour can be monitored, understood, and multiple treatment options can be investigated concurrently. 2D in vitro culture models albeit, easily established and reproducible, fail to replicate the in-vivo tissue architecture. The development of 3D cell culture models, particularly glioma spheroids or neurospheres, have thus provided an opportunity to study tutor progression over time and with minimal harm to the patients (3).
Neurospheres

Neurospheres are aggregates of free floating neural stem cells. The neurosphere assay was first reported by Reynolds and Weiss, which analysed the function of non-tutor neural stem cells derived from the adult mouse brain (4). These nerurspheres indicated mature classes of neural cell types, with multi lineage differentiation once translated in-vivo. Human neurons-here formations was then established using a selection go neural stem cells with the CNS-stem cell marker CD133 (5,6).
Glioma spheroids
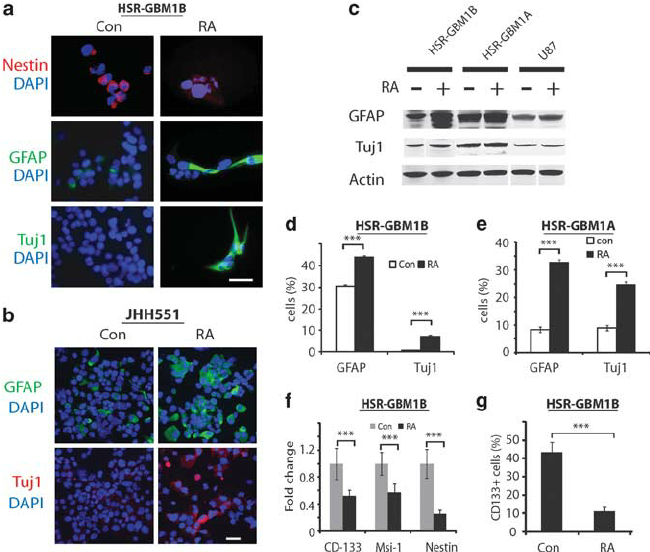
Using these methods, Dirks et al, proceeded to develop glioma spheroids or neurospheres from human gliomas. The CD133 marker positive neural stem cells facilitated the neurosphere formation, and indicated cancer stem cell (CSC) like behaviour with similar capacity for self renewal, proliferation and differentiation (8). Cancer stem cells thus cultivated as neurospheres represent a more reliable model for glioblastoma research when compared with standard serum cultures. These glioma spheroids indicated a similar genotype, gene transcription and biological profile to that of parent cancer, thus affirming is ability to accurately represent gliomas in-vitro. Neurospheres can therefore be used in stem cell specific therapeutic targets and incorporated in assay testing drug efficacy of potential targets (9).
References
1. Stupp, R., Mason, W. P., van den Bent, M. J., Weller, M., Fisher, B., Taphoorn, M. J., et al. (2005). Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 352, 987–996.
2. Rybinski, B., and Yun, K. (2016). Addressing intra-tumoral heterogeneity and therapy resistance. Oncotarget 7, 72322–72342.
3. Sivakumar H, Devarasetty M, Kram DE, Strowd RE and Skardal A (2020) Multi-Cell Type Glioblastoma Tumor Spheroids for Evaluating Sub-Population-Specific Drug Response. Front. Bioeng. Biotechnol. 8:538663.
4. Kempermann, Gerd. Adult Neurogenesis. Oxford University Press, 2006, p. 66-78.
5. Reynolds BA, Weiss S. (1992) Generation of neurons and astrocytes from isolated cells of the adult mammalian central nervous system. Science. 255:1707–10.
6. Lois C, Alvarez-Buylla A. Long-distance neuronal migration in the adult mammalian brain. (1994) Science. 264: 1145-8.
7. Suhonen JO, Peterson DA, Ray J, Gage FH. (1996). Differentiation of adult hippocampus-derived progenitors into olfactory neurons in vivo. Nature. 383: 624-7.
8. Singh SK, Clarke ID, Terasaki M et al.(2003) Identification of a cancer stem cell in human brain tumors. Cancer Res. 63:5821-8.
9. Ishiguro T, Ohata H, Sato A, Yamawaki K, Enomoto T, Okamoto K. (2017). Tumor-derived spheroids: Relevance to cancer stem cells and clinical applications. Cancer Sci. 108(3):283-289.
10. Soubéran, Aurélie, and Aurélie Tchoghandjian. 2020. “Practical Review on Preclinical Human 3D Glioblastoma Models: Advances and Challenges for Clinical Translation” Cancers 12, no. 9: 2347.
