A Living Breathing Human Lung On A Microchip
Modern drug discovery processes have encountered major setbacks over the past decades, despite technological advances in analytical tools and the development of research model. This is primarily due to the lack of predictive models that reliably mimic the complex structure and function of living tissues and organs. Although three-dimensional (3D) cell culture models have made advances in improving the reliability of research models, they are still unable to fully recapitulate the essential architecture and spatial arrangement of multiple tissue types, which significantly affect physiological functions (1,2)
The human lung, and lung cancer
The human lung performs necessary functions for survival such as gas exchange and protecting our body from external hazards (3). In 2020, lung cancer reported the highest mortality rate (4). Tumor cells typically grow in 3D configurations. The surrounding tumor microenvironment is composed of non-tumor cells, and extracellular matrix (ECM).
Within this dynamic microenvironment, tumor cells face hard growth conditions that include low oxygen exposure and nutrient levels and are susceptible to cell-cell interactions and cellular signals from surrounding non- tumor cells (5).
As an attempt to replicate such dynamic conditions in an efficient, reproducible manner, most lung cancer models now employ organ-on-a-chip (OoC) platforms for drug toxicity testing as well as for the investigation of novel therapeutics (4). More specifically, the lung-on-a-chip platform comprises of a microfluidic device produced using human lung and blood vessel cells placed in two layers across a porous flexible boundary.
As the lung tissue cells are exposed to air, a nutrient rich medium flows through the capillary channel to mimic blood circulatory movement, and the cyclic mechanical stretching created by a vacuum applied to the chambers next to the cell culture channel mimics breathing (6).
OoC platforms for lung cancer models
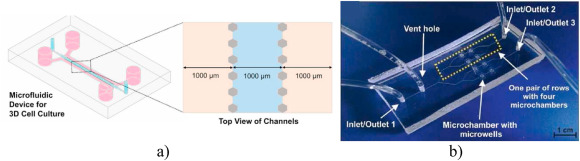
Among the more recent OoC platforms developed for lung cancer are microfluidic devices to study the potential of peptide P1 as possible therapeutic avenue. Cancer cells were embedded in collagen-1 hydrogel and then inserted into microfluidic device to form spheroids (7). Other models include similar devices but with indirect co-culture conditions using conditioned medium of human amniotic membrane-derived mesenchymal stem cells (AMMSCs), or heat-treated AMMSCs. Heat treatment caused a reduction in cell proliferation and spheroid size, and P1 peptide was found to be more cytotoxic to the tumor spheroids (8).
Other studies report the use of microfluidic chips to investigate a photodynamic therapy, which has shown to be effective in selectively targeting tumor cells (9). In these studies, microwells were incorporated to produce cancer spheroids. Microfluidic platforms have also shown to be successful in replicating the in vivo environment of lung cancer to investigate the cytotoxic effects of various drugs in both 2D cultures and 3D cultures on the chip under static and dynamic flow conditions.
In this regard, dynamic flow indicated the best culture condition to evaluate cellular response to drugs. The available lung-on-a- chip models have shown to be effective in producing on-chip lung spheroids without a scaffold as well as with a scaffold such as hydrogels (7-9). The lung cancer spheroids produced indicated uniform size and shape, and reproducibility across several cell lines. Thus, proving to be the next stage in 3D cell culture models for cancer related research.
References
- Horvath P, Aulner N, Bickle M, Davies AM, Nery ED, Ebner D, et al. Screening out irrelevant cell-based models of disease. Nat Rev Drug Discov (2016) 15(11):751–69.
- Scannell JW, Blanckley A, Boldon H, Warrington B. Diagnosing the decline in pharmaceutical R&D efficiency. Nat Rev Drug Discov (2012) 11(3):191–200.
- Wang Y, Tang Z, Huang H, Li J, Wang Z, Yu Y, Zhang C, Li J, Dai H, Wang F, Cai T, Tang N. (2018) Pulmonary alveolar type I cell population consists of two distinct subtypes that differ in cell fate PNAS 115:2407–2412.
- Carvalho V, Bañobre-López M, Minas G, Senhorinha F.C.F. Teixeira, Lima R, Rodrigues R. The integration of spheroids and organoids into organ-on-a-chip platforms for tumour research: A review. Bioprinting, Volume 27 (2022)
- Ishiguro T, Ohata H, Sato A, Yamawaki K, Enomoto T, Okamoto K. Tumor-derived spheroids: Relevance to cancer stem cells and clinical applications. Cancer Sci. 2017 Mar; 108(3):283-289.
- Huh D et al. Reconstituting organ-level lung functions on a chip. (2010) Science 328:1662–1668.
- Dhiman N, Shagaghi N, Bhave M, Sumer H, Kingshott P, Rath S.N. Selective cytotoxicity of a novel trp-rich peptide against lung tumor spheroids encapsulated inside a 3D microfluidic device, Adv. Biosyst. 4 (2020), 1900285.
- Dhiman N, Shagaghi N, Bhave M, Sumer H, Kingshott P, Rath S.N. Indirect co-culture of lung carcinoma cells with hyperthermia-treated mesenchymal stem cells influences tumor spheroid growth in a collagen-based 3-dimensional microfluidic model, Cytotherapy 23 (2020) 25–36.
- Zuchowska A, Jastrzebska E, Chudy M, Dybko A. 3D lung spheroid cultures for evaluation of photodynamic therapy (PDT) procedures in microfluidic Lab-on-a-Chip system, Anal. Chim. Acta 990 (2017) 110–120.
- Mani V, Lyu Z, Kumar V, Ercal B, Chen H, Malhotra S.V, Demirci U. Epithelial-to-Mesenchymal transition (EMT) and drug response in dynamic bioengineered lung cancer microenvironment, Adv. Biosyst. 3 (2019).
